Silent Sabotage: How Cancer Hijacks Immune Cells from Within
Curious how cancer cells weaken the immune system from within? Discover a groundbreaking study revealing hidden mitochondrial tactics now!

Mitochondrial transfer between cancer and immune cells has been identified by researchers as a significant contributor to immune evasion in tumors.
A functional immune system plays a vital role in detecting and eliminating cancerous growths. Through immunotherapy, this natural defense is supported by encouraging immune cells to recognize and target tumor cells more effectively. Despite these advancements, many cancers adopt strategies that allow them to escape immune surveillance, contributing to treatment resistance. A deeper understanding of the underlying molecular processes driving this immune evasion remains essential for refining therapeutic approaches.
Within the tumor microenvironment—a complex cellular landscape surrounding malignant tissue—interactions between cancer cells and immune defenders are heavily influenced. Manipulation of this environment by cancer cells has been shown to suppress the activity of tumor-infiltrating lymphocytes, which are typically involved in tumor destruction. Mitochondria, frequently referred to as the “powerhouse of the cell,” serve as key players in cellular energy production and are deeply involved in metabolic changes within both cancer cells and immune responders. Nonetheless, the precise mechanisms through which mitochondrial alterations affect this environment are still not fully clarified.
Emerging Findings on Mitochondrial Dysfunction in Cancer
New insights have been reported regarding the role of mitochondrial dysfunction in enabling cancer to evade immune responses. This advancement in understanding was made possible through the collaborative efforts of researchers from Okayama University, Japan, and the Chiba Cancer Center Research Institute. The study, led by Professor Yosuke Togashi and published in Nature on January 22, 2025, has highlighted mitochondrial transfer as a central mechanism behind immune evasion in tumors.
“We have discovered mitochondrial transfer as one of the key mechanisms of immune evasion. Our research adds a new dimension to the understanding of how tumors resist immune responses, potentially leading to the development of more comprehensive and tailored approaches in treating different cancers.”
Professor Togashi
Mitochondria, known for producing cellular energy, contain their own DNA (mtDNA). This genetic material, essential for energy-related protein synthesis, is vulnerable to damage. Mutations in mtDNA have been associated with enhanced tumor growth and spread. In this study, tumor-infiltrating lymphocytes (TILs) collected from cancer patients were found to possess identical mtDNA mutations as those present in the surrounding cancer cells. This discovery suggested a direct exchange of mitochondria between these cell types.
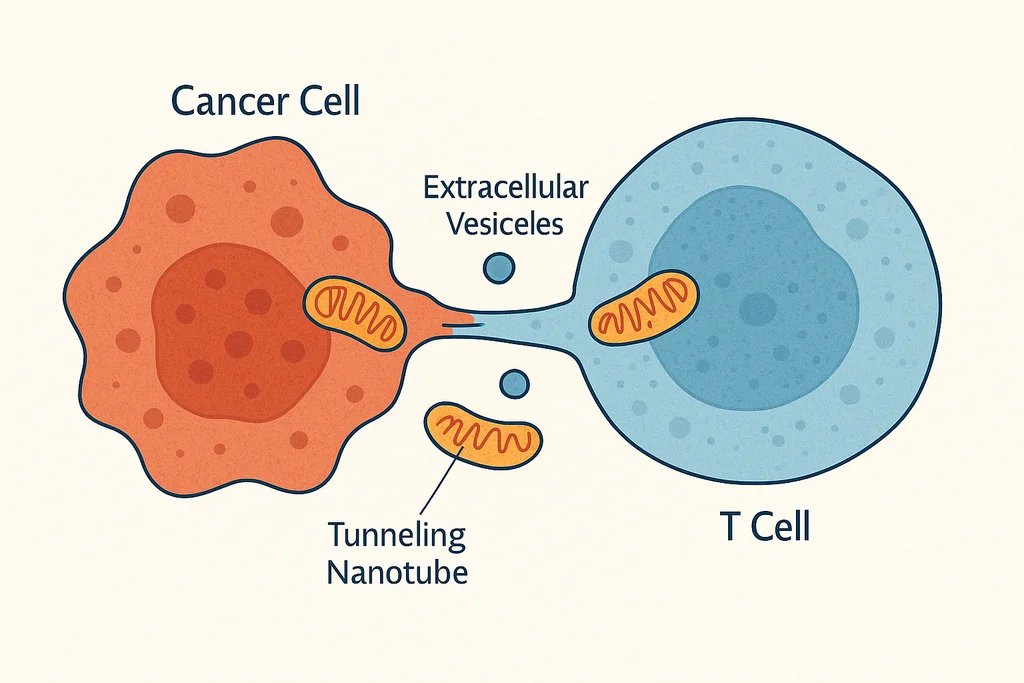
By utilizing fluorescent markers, mitochondrial transfer was observed through both tunneling nanotubes—thin, tube-like structures connecting cells—and extracellular vesicles. Once inside immune cells, mitochondria originating from cancer cells progressively replaced the native ones. This led to a condition termed “homoplasmy,” where all copies of mtDNA within a cell became identical, mirroring the mutations carried by the tumor.
Mechanisms That Shield Transferred Mitochondria in Cancer
Under typical conditions, damaged mitochondria in tumor-infiltrating lymphocytes (TILs) are eliminated through a natural quality control process known as mitophagy. In contrast, mitochondria received from cancer cells have been observed to resist this degradation. Research has shown that molecules capable of suppressing mitophagy are co-delivered alongside the transferred mitochondria. This protective mechanism allows foreign mitochondria to persist within immune cells, leading to mitochondrial dysfunction.
Consequences of this dysfunction include diminished cellular proliferation, altered metabolism, increased oxidative stress, and weakened immune function. In preclinical models, TILs affected in this way also exhibited reduced responsiveness to immune checkpoint inhibitors, which are commonly used in modern immunotherapy.
Through the identification of mitochondrial transfer as an immune evasion strategy, new opportunities have emerged for enhancing therapeutic outcomes. Interrupting this transfer process may offer a path toward restoring immune cell function and improving the effectiveness of treatment—particularly for cancers that currently resist standard interventions.
The burden of cancer, often compounded by high treatment costs and adverse effects, underscores the importance of more targeted and successful therapies. An approach focused on preventing mitochondrial transfer may reduce treatment resistance and support better outcomes.
“Existing cancer treatments are not universally effective, and there is a pressing need for new therapies that can overcome resistance mechanisms. Developing drugs that inhibit mitochondrial transfer between cancer cells and immune cells may enhance the efficacy of immunotherapies, thereby providing personalized treatment options for patients with cancers that are resistant to current therapies.”
Professor Togashi
This breakthrough offers a deeper understanding of cancer biology and may guide the development of more precise and powerful treatments in the future.
https://www.nature.com/articles/s41586-024-08439-0
Summary
Cancer cells within the tumor microenvironment evade immune responses, particularly T cell attacks, by transferring mitochondria carrying mutated mitochondrial DNA (mtDNA) to tumor-infiltrating lymphocytes (TILs). These transferred mitochondria resist normal degradation due to attached mitophagy-inhibiting molecules, leading to the replacement of native mitochondria in TILs. As a result, T cells develop metabolic dysfunction, senescence, and impaired immune function. This mitochondrial transfer weakens antitumor immunity and is associated with poor responses to immune checkpoint inhibitors, revealing a novel mechanism of immune evasion and a potential target for improving cancer immunotherapy.
